Neuroendocrine Tumor (NET) Cancer
What is Neuroendocrine Tumor Cancer ?
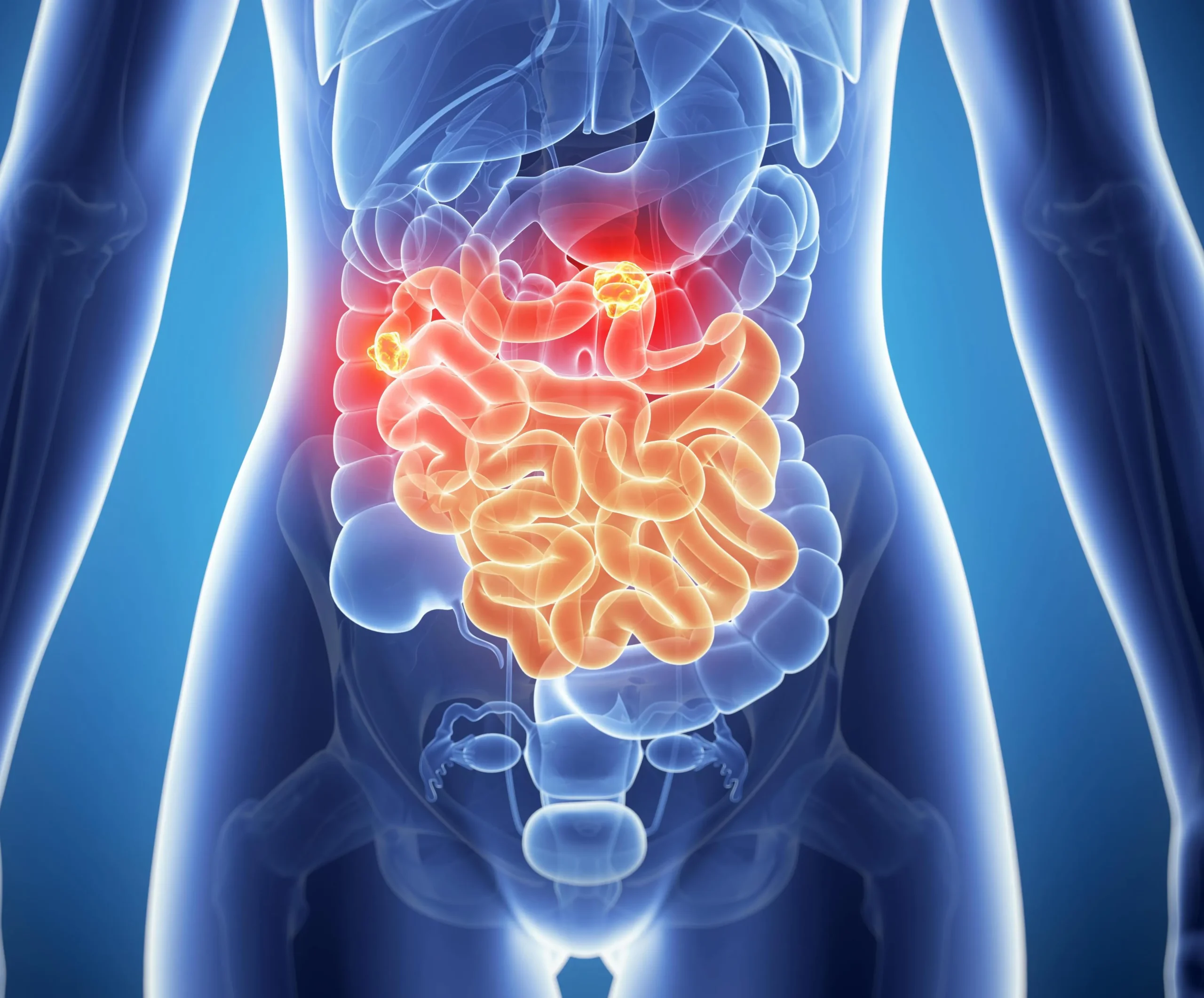
Neuroendocrine Tumors are a diverse group of growths that develop from neuroendocrine cells scattered throughout the body, playing a crucial role in hormonal balance. Such neoplasms could develop in organs like the pancreas, gastrointestinal tract, lung, and other sites with neuroendocrine cells. Neuroendocrine tumors are specified by hormones that they can secrete, thus generating diverse symptoms and complications. Neuroendocrine tumors are relatively rare, though their incidence is increasing with time, presenting varied and challenging diagnostic and therapeutic obstacles because of their heterogeneity & broad clinical spectrums.
Depending on these tumors’ location, size, and degree of hormone secretion, their symptomatology can vary widely. Common symptoms include abdominal pain, flushing, diarrhea, wheezing, unexplained weight loss, palpable masses, and fatigue. In some cases, excessive hormone production by tumors can cause specific syndromes, such as carcinoid syndrome.

Neuroendocrine Tumor Cancer Treatments
Neuroendocrine tumors (NETs) are a diversified group of growths that appear and behave clinically differently. Treatment modalities for Neuroendocrine tumors vary greatly depending on the grade, stage, location, and presence of secreted hormones.
Our oncologists, surgeons, gastroenterologists, and endocrinologists must make comprehensive treatment plans according to individual patient needs.
Surgery
Surgical removal is the primary treatment for localized Neuroendocrine tumors, aiming to remove the cancer and potentially achieve a cure ultimately.
Different surgical options include tumor excision, pancreaticoduodenectomy (Whipple’s procedure), liver resection for metastases, or debulking surgery to palliate symptoms that improve quality of life.
Medical Therapies
Neuroendocrine tumors that cannot be surgically removed or have spread are treated with medical therapies aimed at controlling tumor growth, relieving symptoms, and improving quality of life.
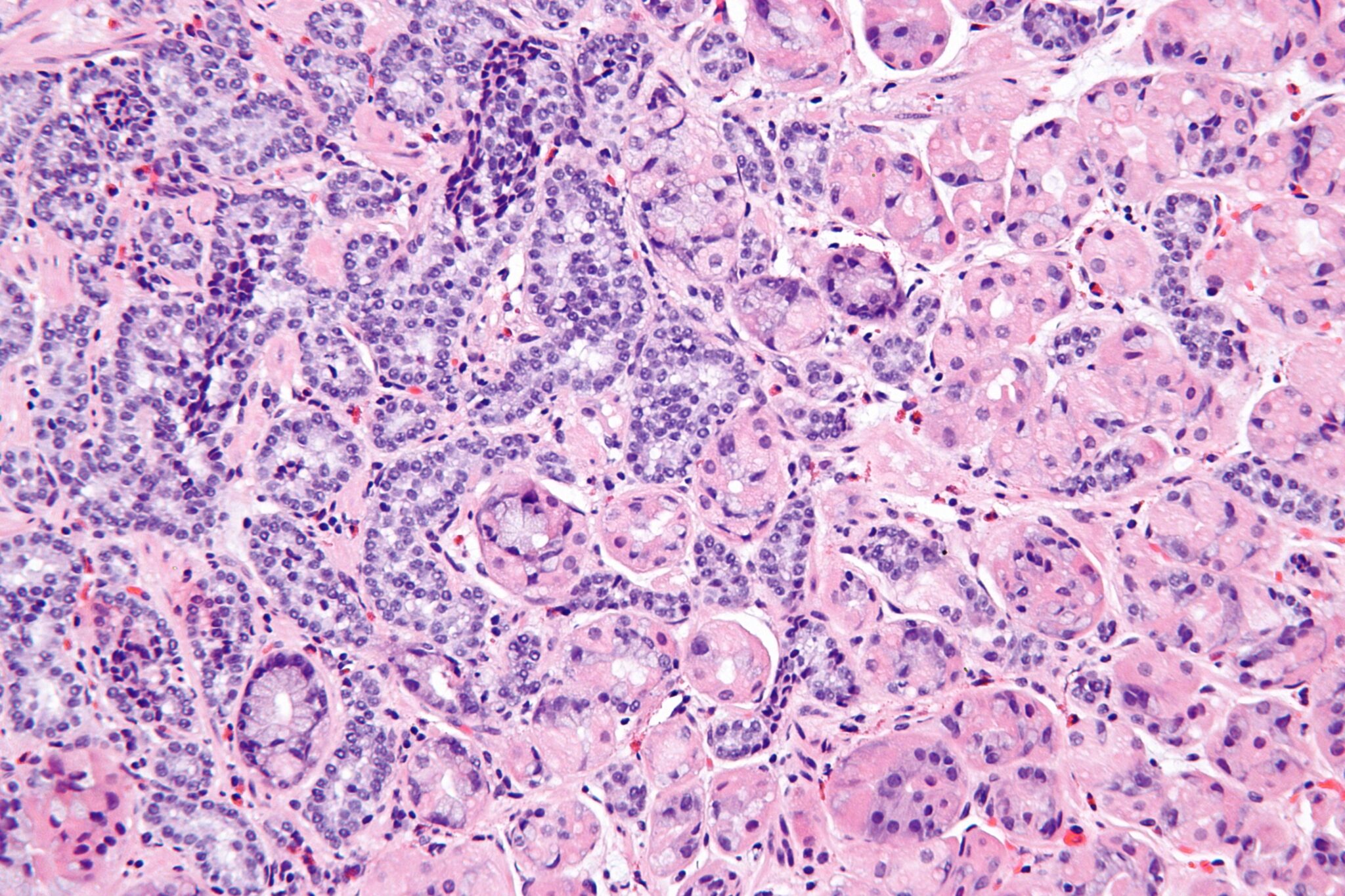
Neuroendocrine Tumor Diagnosis
Neuroendocrine tumor diagnosis mainly depends upon a patient’s typical and reported signs and symptoms. It can be a single or a group of symptoms. Various techniques, including blood tests, imaging scans, genetic evaluation, and pathological studies, have been performed for the neuroendocrine tumor diagnosis.
Biochemical Markers:
– Some common biochemical markers are serum chromogranin A and urinary levels of 5-hydroxyindoleacetic acid.
– Elevated serum chromogranin A (CgA) levels suggest neuroendocrine tumors lack specificity.
– Carcinoid syndrome can be suggested by increased urinary excretion of 5-hydroxyindoleacetic acid (5-HIAA).
– In some cases, specialists may measure other hormone levels such as insulin, glucagon, and gastrin, which can be a specific tumor type.
Imaging Studies:
Computed Tomography (CT) Scan: Used for initial evaluation, it gives detailed images about the size and location of the tumor.
Magnetic Resonance Imaging (MRI): Superior soft tissue resolution. It is instrumental in evaluating liver metastasis.
Somatostatin Receptor Scintigraphy (Octreotide Scan): The technique helps to detect somatostatin receptor-positive tumors, thus assisting in staging and localization.
Positron Emission Tomography (PET) Scan: Radiolabeled tracers detect tumor activity. This method is precious for staging disease and identifying metastases.
Endoscopic Procedures: Upper Endoscopy allows visualization and biopsy of tumors within the upper gastrointestinal tract.
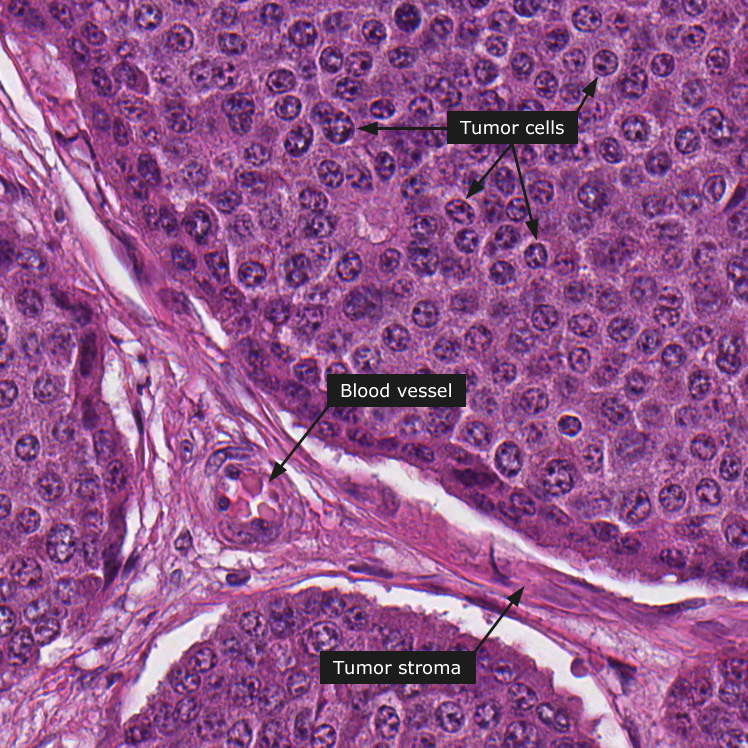
How Neuroendocrine Tumor Cancer Develops
Neuroendocrine tumors (NETs) originate in neuroendocrine cells spread throughout the body. These cells control hormone production and release. Many factors influence the development of Neuroendocrine tumors, and although the cause remains unknown, several things are known to contribute to their development.
Genetic predisposition plays a significant role, especially in specific inherited conditions like multiple endocrine neoplasia type 1 (MEN1), neurofibromatosis type 1 (NF1), and von Hippel-Lindau (VHL) disease, which heighten an individual’s risk. Likewise, exposure to toxins and carcinogens in our environment can also increase the chances of developing tumors. Furthermore, there are cases where Neuroendocrine tumors temporarily develop without any known genetic or environmental link.
Common Signs and Symptoms of Neuroendocrine Tumors Cancer
- The signs of neuroendocrine tumors depend on their location, size, and hormone secretion activities.
- Some common symptoms include abdominal pain, wheezing, fatigue, unintended weight loss, and palpable masses.
- In some instances, patients may experience specific syndromes if their tumors produce excessive hormones, such as carcinoid syndrome.
- The symptoms of this syndrome include flushing of the face and neck, diarrhea, wheezing, cough, and chest pain, alongside other features related to cancerous tissue growth on the heart.
- On top of this pancreas, Neuroendocrine tumors can lead to hormonal excess evident through symptoms like hypoglycemia(insulinomas) or peptic ulcers(para-gastrinoma).
Facts About Neuroendocrine Tumor Cancer
Neuroendocrine tumors are neoplasms originating from the cells of the neuroendocrine system, which produce hormones to regulate various bodily functions.
Their classification is dependent on the site of origin and hormone production.
They include pancreatic NETs, gastrointestinal Neuroendocrine tumors(carcinoids), and lung Neuroendocrine tumors(typical and atypical carcinoids).
The causes are unknown, but genetic predisposition, environmental factors, and specific syndromes, including multiple endocrine neoplasia type 1, are observed.
Tumor development results from mutation of tumor suppressor genes.
The early symptoms depend on the location of the tumor, its size, and the amount of hormone it secretes.
Carcinoid syndrome may present with flushing, diarrhea, bronchospasm, and carcinoid heart disease.